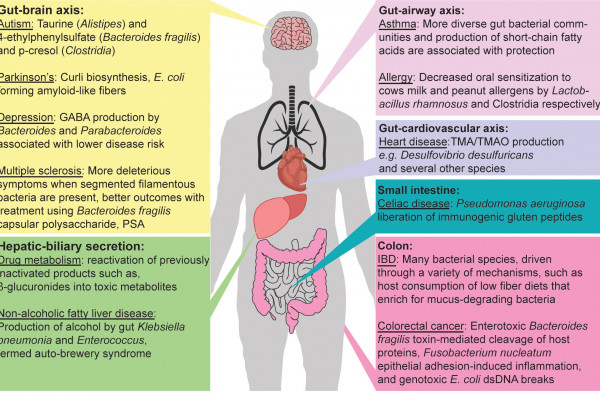
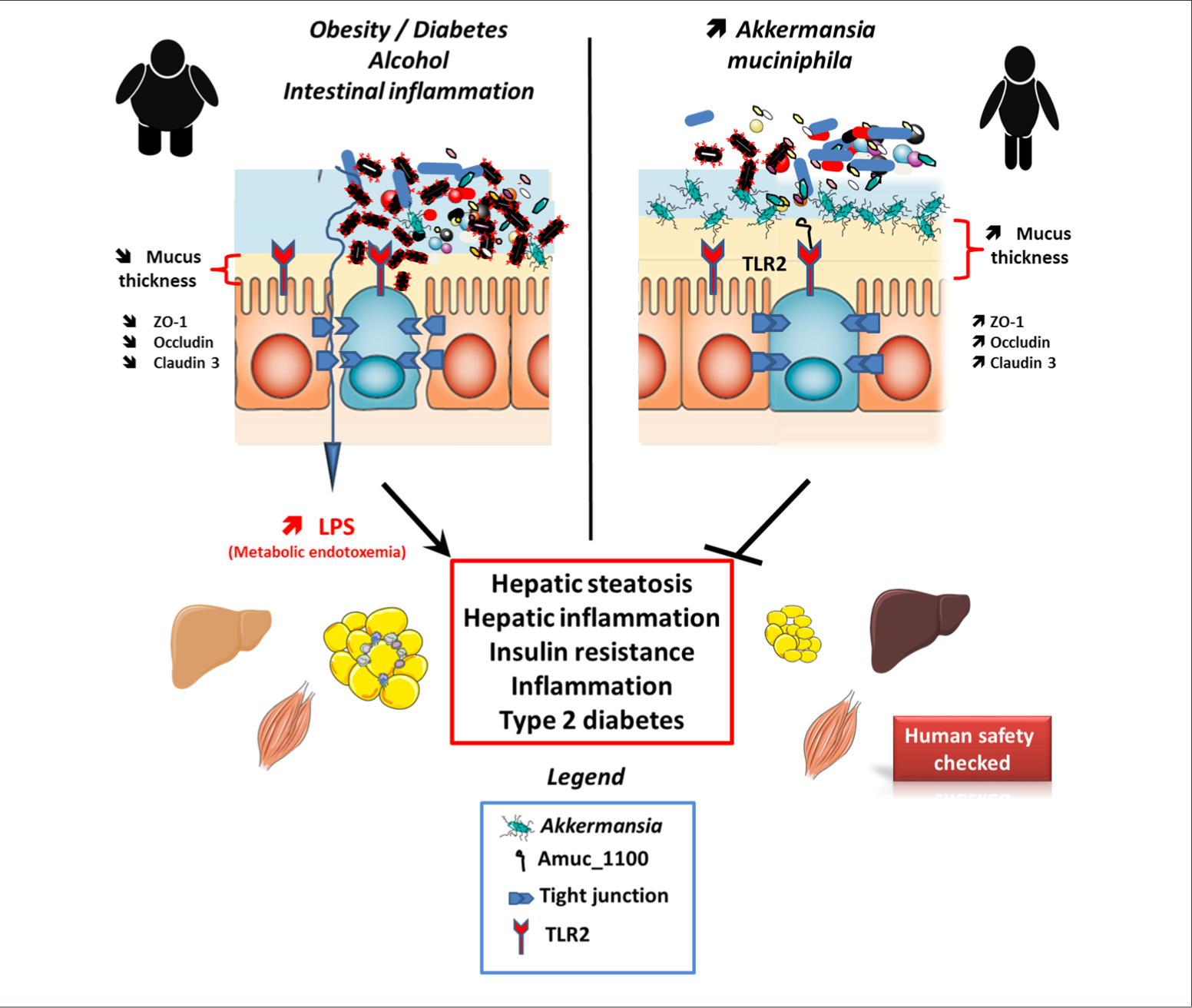
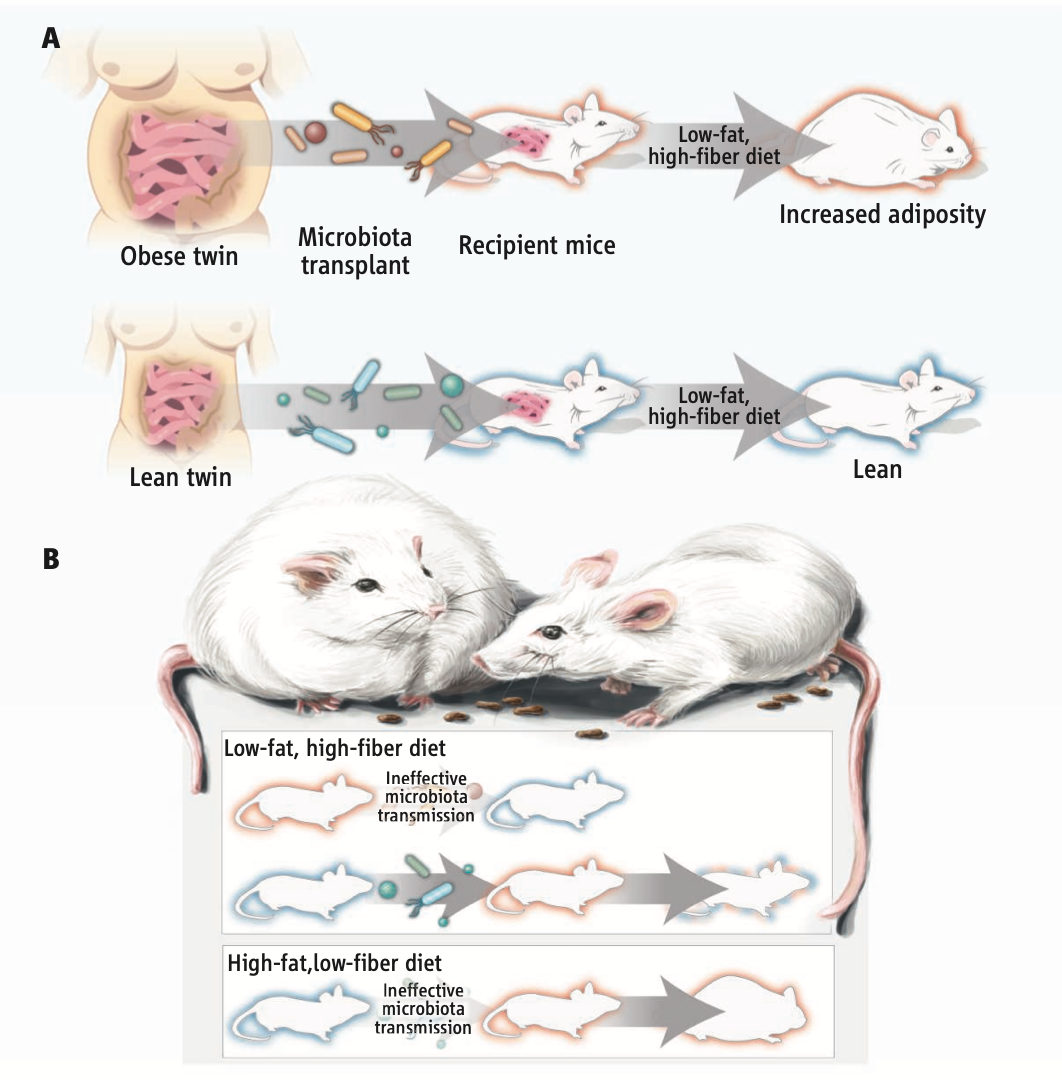
The gut microbiota is a key player involved in health and diseases. Approximately 1014 bacteria and archaea of more than 1,000 species exist in the human gastrointestinal tract; together, these are known as the gut microbiota. The impact of the gut microbiome on health has been a major focus of interest for the past couple of decades, since an adequate gut microbiota and probiotic supplementation have positive effects on many health conditions, including type 2 diabetes, cardiovascular diseases, and immune and infectious diseases. The role of the gut microbiome in affecting the wellbeing of individuals is encouraging researchers to find new treatments for different health conditions, such as obesity and weight gain. A reciprocated relationship exists between the gut flora and diet, whereby dietary factors regulate the role and structure of the microbiota. of nutrients and have potential consequences on host physiology.
Professor Dr Amandine Everard is assistant professor of Metabolism and Nutrition, researcher from the Belgian Fund for Scientific Research (FNRS) and group leader in the Metabolism and Nutrition lab at the Louvain Drug Research Institute (LDRI) from the UCLouvain, Brussels, Belgium. She is WELBIO investigator (Walloon Excellence in Life Biotechnology). Her main topic of interest in research is to study how gut microbes can impact on metabolic disorders, such as obesity, type 2 diabetes. More specifically, she is investigating the interactions between the gut microbiota, the intestine and the brain in the context of obesity, type 2 diabetes and metabolic diseases.
Title Image credit : Robert W. P. Glowacki, Eric C. Martens, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons